by
Lauren Dubinsky, Senior Reporter | May 01, 2018
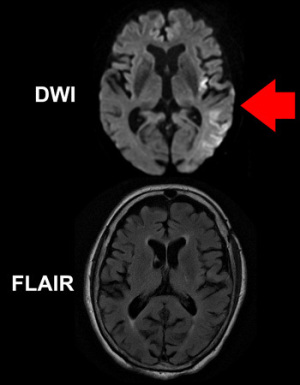
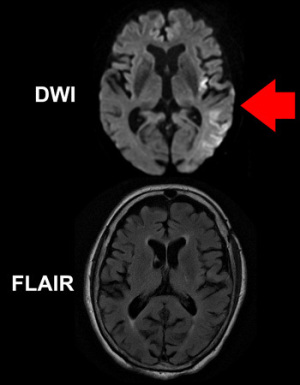
The mismatch between the two
images implies the patient was imaged within
4.5 hours of symptom onset.
Courtesy of Ona Wu
For up to 25 percent of stroke patients, their early symptoms go unnoticed, and that often prevents them from receiving tPA treatment. But researchers at MGH may have found a way around that.
“So many patients don't qualify for treatment because they arrive too late and this might be something we can change in the future,” Dr. Lee Schwamm, co-lead and corresponding author of the study, told HCB News.
For patients whose initial symptoms were not witnessed and it’s been over 4.5 hours since they were last known to be well, tPA is not approved for use. This study used MR-based imaging technologies to identify patients likely to be within 4.5 hours of stroke onset, even if their initial symptoms were not witnessed.



Ad Statistics
Times Displayed: 75267
Times Visited: 5317 MIT labs, experts in Multi-Vendor component level repair of: MRI Coils, RF amplifiers, Gradient Amplifiers Contrast Media Injectors. System repairs, sub-assembly repairs, component level repairs, refurbish/calibrate. info@mitlabsusa.com/+1 (305) 470-8013
Schwamm and her team recruited 80 patients with ischemic stroke that imaging confirmed was unwitnessed at its onset. It was less than 24 hours since they were last known to be well.
Study eligibility was determined by a mismatch between two types of MR imaging studies — FLAIR, which typically only shows stroke effects on brain tissue after several hours of reduced blood flow, and the diffusion-weight imaging (DWI) technique that is very sensitive to changes beginning in the first minutes or hours after stroke onset.
Ona Wu, the co-lead author, explained that brain tissue that is abnormal on DWI but not yet abnormal on FLAIR has been seen in patients that were four hours or less after known symptom onset. That shows the evolution of tissue as the stroke progresses in the first few hours.
The team used that pattern to select patients for tPA treatment and called the method quantitative DWI FLAIR Mismatch (qDFM). The selected patients were likely to be similar to patients with known symptom onset who benefited from tPA because their strokes had not yet caused irreversible injury.
The team found that the outcomes for the study participants who received tPA on the basis of qDFM were similar to those who previously received tPA within 4.5 hours of witnessed strokes. In addition, over 70 percent of the study participants experienced wake-up strokes.
“We hope that a large randomized study of [patients who meet] these criteria will be performed to see if this treatment can be effective for patients who present with wake-up stroke,” said Schwamm.
The team also hopes to conduct a follow-up, placebo-controlled trial that will compare MR with CT imaging for identifying patients with unwitnessed strokes who could safely and effectively be treated with tPA.
Back to HCB News