by
Lauren Dubinsky, Senior Reporter | December 14, 2017
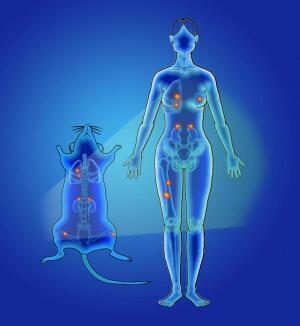
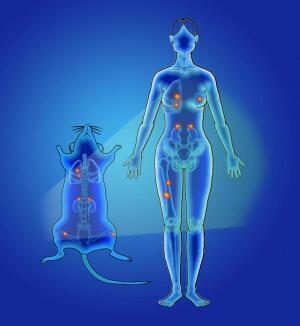
human breast cancer cells in a
mouse model were tracked with
novel rare earth nanoscale
probes injected intravenously
Researchers at Rutgers University have invented a faster, more accurate method for detecting and tracking cancer using light-emitting nanoprobes.
In a study published in
Nature Biomedical Engineering, they proved that this method is superior to MR and other cancer surveillance technology like PET and SPECT.
"The main difference is that our method has a much higher resolution so we can image smaller clusters of cancer cells down to tens and hundreds of micrometers, whereas the PET and SPECT methods can only identify disease at the level of millimeters," Prabhas V. Moghe, corresponding author of the study, told HCB News.



Ad Statistics
Times Displayed: 75267
Times Visited: 5317 MIT labs, experts in Multi-Vendor component level repair of: MRI Coils, RF amplifiers, Gradient Amplifiers Contrast Media Injectors. System repairs, sub-assembly repairs, component level repairs, refurbish/calibrate. info@mitlabsusa.com/+1 (305) 470-8013
Another key difference is that while PET and SPECT methods are not used for real-time disease monitoring, the nanoparticle method can be used for real-time fluorescence-guided surgeries.
For the preclinical study, mice were injected with the nanoprobes, which emit short-wave infrared light as they travel through the bloodstream. The researchers found that this method can detect tiny tumors, even tracking them in multiple organs.
They also showed that the nanoprobes were significantly faster than MR at detecting the minute spread of tiny lesions and tumors in the adrenal glands and bones of mice. For humans, that means this method can detect cancer months earlier than other approaches.
The nanoparticle technology could be capable of detecting and tracking over 100 types of cancer and may be available within the next five years. Prabhas has already assembled a team to guide them along the commercialization process.
"We have already demonstrated good safety profiles for the probes in vivo," she said. "The next step to move toward human clinical applications requires FDA regulatory approval to get these on the market — expect this to take 2-3 years, depending on the specific application."